Featured Photo from CDC.gov
On July 23, 2022, the World Health Organization declared monkeypox a public health emergency of international concern which means the United States is included in a list of places where human-to-human transmission of monkeypox is occurring.
For now, monkeypox is occurring in high-risk groups, particularly men who have sex with men.
It is important to note that monkeypox can impact anyone who comes into contact with it, not just people in high risk groups.
According to the American Academy of Dermatology “those who have any sort of close personal contact with people with monkeypox could potentially also be at risk for the disease.”
Here’s what you need to know about monkeypox
What Causes Monkeypox?
Monkeypox is caused by a virus- the same family of viruses that causes smallpox. Monkeypox is not as severe as smallpox. Fortunately monkeypox is rarely a life-threatening illness.
Monkeypox was first discovered in the 1950s. And although the name has the word “monkey” in it, experts aren’t sure of the original source of the virus.
The first human case of monkeypox was in 1970. Because this is not a novel virus, fortunately there is a vaccine already in place.
How is Monkeypox Spread?
Monkeypox is generally spread through direct close contact, including intimate contact. The disease can also be spread through droplets from face-to-face contact with an infected person.
It is possible to get monkeypox from touching items that have been contaminated with the rash or body fluids including sheets and towels. It is possible for a pregnant woman to spread the virus to their unborn child through the placenta.
What is the incubation period?
Monkeypox has an incubation period of one to two weeks.
How Does Monkeypox Present?
Monkeypox can start with a fever. People often have swollen lymph nodes as well. People can also have headaches, muscle aches, back pain, chills, fatigue, exhaustion. There is also a characteristic rash that can happen with monkeypox. Some people can present only with skin findings.
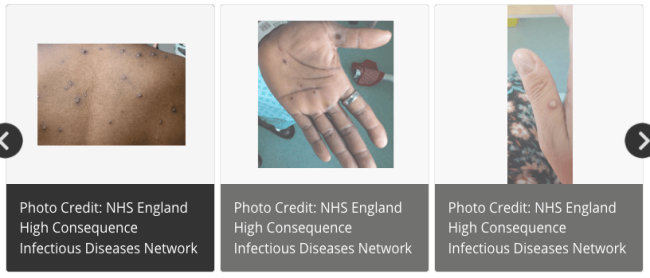
What Can Monkeypox Look Like on the Skin?
1. Pustules with surrounding redness
Monkeypox cases classically present with pimple-like lesions. They can look ike pustules with redness around them. The typical evolution of the rash is that the pustules progress to blisters that eventually scab over.
Monkeypox can start as a genital rash, but the lesions can pop up anywhere including the face, eyes, and lips.
The rashes in the genital area can be painful and can be associated with rectal pain and even rectal bleeding.
According to the CDC, the illness of monkeypox lasts two to four weeks and people are contagious “until the rash has fully healed and a fresh layer of skin has formed.”
Keeping an eye out for blistering rashes is important, especially if you feel unwell or have a fever. If you have a blistering rash that is unexplained, or if you have any systemic illness with any rash that is blistering, you need to keep contact to a minimum until it is assessed by a healthcare professional.
2. Swollen lymph nodes along with a rash are more suggestive of monkeypox
A prominent feature of monkeypox, and a sign that helps distinguish monkeypox from many other viral illnesses, is the presence of painful, swollen lymph nodes.
Lymph nodes become enlarged usually at the time of fever and can become involved a few days before the appearance of any rash.
It is important to consider monkeypox and have an evaluation if you have a rash in the genital area that is associated with any swollen lymph nodes.
What Other Diseases Can Look like Monkeypox?
Fortunately there is no need for panic. Although monkeypox is now a public health emergency, most skin rashes are not because of monkeypox. Many diseases have skin findings that look similar. Monkeypox has even been described by doctors as a ‘mimicker’ illness. Here are some other conditions that look like monkeypox, but aren’t:
- Other viral infections. Other viral illnesses like herpes, varicella (the virus that causes chickenpox), shingles (reactivation of chickenpox), molluscum virus (commonly seen in kids), and hand-foot-mouth disease are all much more common illnesses that can mimic monkeypox rashes.
- Bullous impetigo: This is a superficial bacterial skin infection with overlying crusted blisters.
- Blistering fungal infections: Fungal infections are usually pink scaling rashes, but occasionally a fungal infection can cause a blistering rash.
- Syphilis: The rash of syphilis can mimic monkeypox. Because monkeypox can be sexually transmitted, other sexually transmitted diseases like syphilis, gonorrhea, or chlamydia can be co-transmitted at the time of contact.
- Contact dermatitis: Irritant and allergic contact dermatitis rashes sometimes develop blisters.
- Folliculitis- infections of hair follicles can develop pustules and could look like monkeypox
Can you spread monkeypox without a rash or without realizing it?
Many viruses can be infectious without showing symptoms. This is a concept we have all become familiar with because of COVID-19. And it is highly likely there are many cases of monkeypox that haven’t been reported.
Now, there are lab tests that can help identify cases. Viral cultures using PCR, similar to the technique used for many COVID-19 tests, are available from the big commercial testing labs in the United States.
While the CDC says, “people who do not have monkeypox symptoms cannot spread the virus to others,” experts caution people may not always recognize early signs of monkeypox as a contagious viral illness.
Can monkeypox be treated?
While there is no treatment specifically for monkeypox, antivirals can be used for cases that are likely to be severe or in certain patients with weakened immune systems.
Is there a Vaccine for Monkeypox?
After the first human cases of monkeypox in 1970, vaccines were developed. Right now there are two monkeypox vaccines available to prevent monkeypox. One is called JYNNEOS (also known as Imvamune or Imvanex) and the other is called ACAM2000.
Because vaccine supply is not widely available, administration of the vaccines is currently being targeted to those at highest risk for catching the disease.
ACAM2000 should not be used in people with compromised immune systems, people with certain skin conditions like eczema or in pregnancy.
To learn more about Monkeypox, watch Dr. Abdelmalek’s segment on ABC News here.